The medical device industry plays a pivotal role in advancing healthcare across the
globe. With products developed and manufactured in one region often being marketed
and sold internationally, it is crucial for medical device companies to understand the
complex web of regulations that govern these products in different parts of the world.
Ensuring that medical devices are safe and effective for patients is paramount. As a
result, medical devices are subject to stringent regulations by various regional
regulatory bodies. In this post, I’ll provide a snapshot of the several regulatory bodies
and requirements.
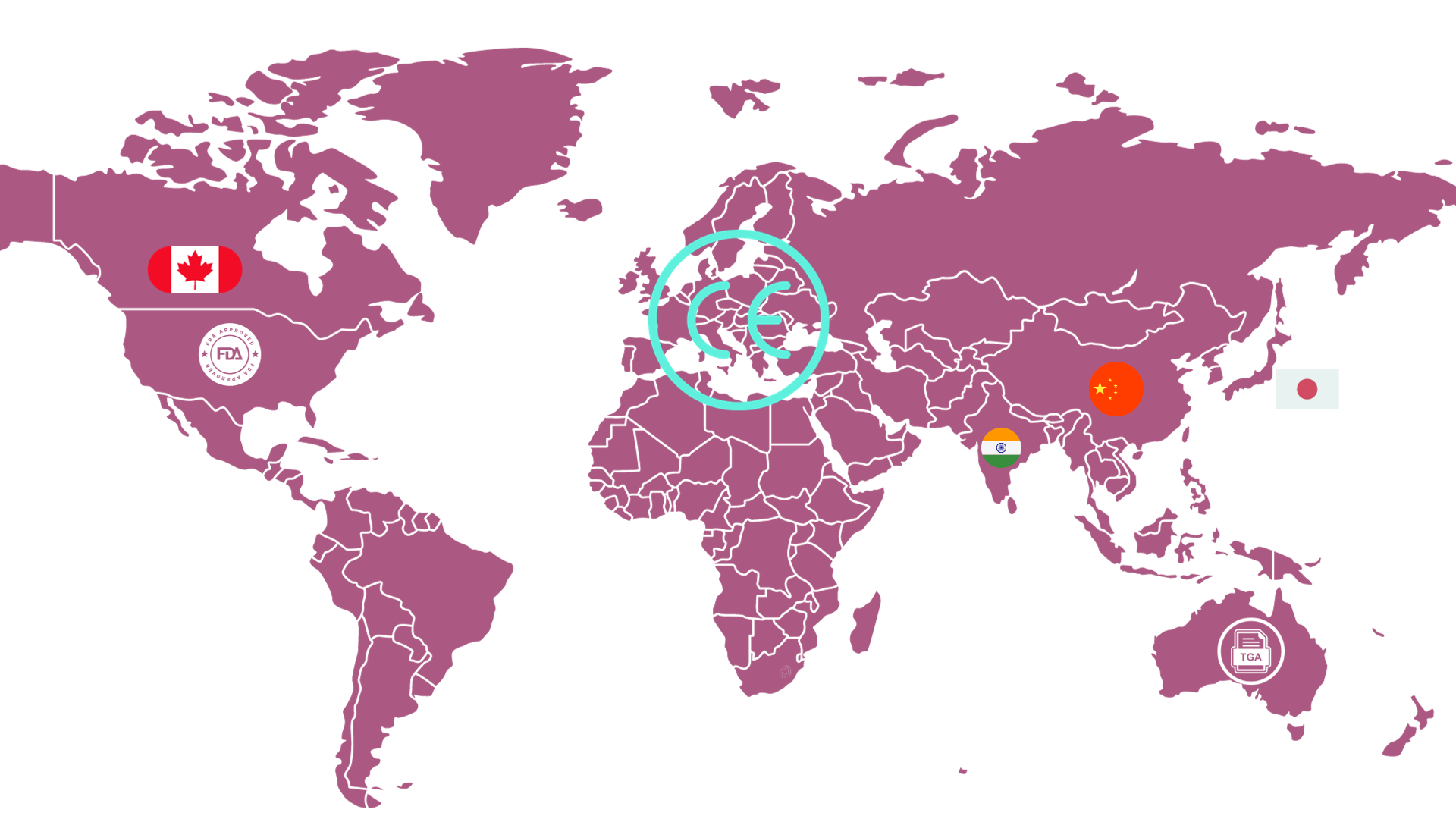
The following are some of the key regulatory bodies for medical devices in different
regions:
• United States: Food and Drug Administration (FDA).
• European Union: European Commission (EC).
• Canada: Health Canada (HC).
• Japan: Pharmaceutical and Medical Devices Agency (PMDA).
• Australia: Therapeutic Goods Administration (TGA).
• China: National Medical Products Administration (NMPA).
• India: Central Drugs Standard Control Organization (CDSCO).
Regulatory requirements
The specific regulatory requirements for medical devices vary depending on the type of
device and the region where it is being marketed. However, some general requirements
apply to all medical devices, such as:
• The device must be safe and effective for its intended use.
• The device must be manufactured in accordance with quality system regulations.
• The device must be labeled accurately and informatively.
• The manufacturer must report any adverse events associated with the device to
the regulatory authority.
Premarket approval
Some medical devices require premarket approval from the regulatory authority before
being marketed. This is typically required for high-risk devices, such as implants and life-sustaining devices.
To obtain premarket approval, the manufacturer must submit a premarket approval
application to the regulatory authority. The application must include technical and
clinical data that demonstrate the safety, performance, and efficacy of the device.
Postmarket surveillance
Once a medical device is marketed, the manufacturer must monitor its safety,
performance, and efficacy. This is known as postmarket surveillance.
The manufacturer must collect and analyze data from postmarket surveillance activities,
such as adverse event reports and customer complaints. This data can be used to
identify and address any safety, performance, or efficacy concerns with the device.
Regulatory requirements in different regions
The following is a brief overview of the regulatory requirements for medical devices in
different regions:
1. USA – Food and Drug Administration (FDA)
• Regulatory Body: The primary body overseeing medical device regulations in
the USA is the Food and Drug Administration (FDA). The FDA regulates
medical devices under the Medical Device Amendments of 1976.
• Classification System: The FDA classifies medical devices into three
categories based on risk: Class I (low risk), Class II (moderate risk), and Class
III (high risk).
• Pre-Market Approval (PMA): For high-risk devices (Class III), manufacturers
typically need to obtain a PMA, which requires rigorous clinical testing and
review.
• 510(k) Clearance: For most Class II and some Class I devices, manufacturers
can seek 510(k) clearance, demonstrating that the device is substantially
equivalent to a device already on the market.
• De Novo request: Provides a marketing pathway to classify novel medical
devices that are usually low risk and provide reproducible controls to manage
those risks,
• Humanitarian Device Exemption (HDE): A marketing application exempt
from effectiveness requirements that is subject to certain profit and use
restrictions.
• Establishment Registration: All facilities producing and distributing devices
must be registered annually with the FDA.
• Quality System Regulation (QSR): Manufacturers must establish and adhere
to quality systems to ensure their products consistently meet regulatory
requirements.
2. EU – CE Marking
• Regulatory Body: In the European Union, the regulatory framework revolves
around obtaining a CE Mark.
• Medical Device Regulations (MDR and IVDR): The EU’s Regulations provide a
modernized and more robust EU legislative framework, ensuring better
protection of public health and patient safety.
• Classification System: Devices are classified into four classes – Class I, IIa, IIb,
and III, ascending in risk.
• Notified Bodies: Unlike the centralized FDA system, the EU relies on Notified
Bodies – independent entities designated by EU countries to assess the
conformity of certain products before being placed on the market.
• Conformity Assessment: Before affixing the CE marking, manufacturers must
undertake a conformity assessment, demonstrating that the device meets all
regulatory requirements.
• Quality management systems (QMS): Must meet ISO 13485.
3. Canada: Health Canada
• Regulatory Body: Health Canada Medical Devices Bureau (MDB) regulates
medical devices in Canada under the Medical Devices Regulations (MDR).
• Classification System: Health Canada classifies medical devices into four risk
categories: Class I (low risk), Class II (medium risk), Class III (high risk), and
Class IV (implantable).
• Conformity Assessment: Class III and Class IV devices require premarket
approval.
4. Japan: PMDA
• Regulatory Body: The PMDA, in collaboration with the Ministry of Health,
Labor, and Welfare (MHLW), manages the country’s medical device
regulations.
• Device Classification: Devices are classified into Classes I to IV based on risk,
with IV being the highest.
• Pre-market Certification/Approval: Depending on the device class, either
certification (by registered certification bodies) or approval (by the MHLW) is
needed. Extensive technical documentation and clinical data must be
submitted to PMDA for review.
• Quality Management System (QMS) Audit: Manufacturing quality control
and design/development management systems must comply with Japanese
regulations based on ISO 13485 and ISO 14971. Labeling must include
indications for use in Japanese. Post-market surveillance is also mandated.
5. Australia – Therapeutic Goods Administration (TGA)
• Regulatory Body: The TGA oversees the safety, effectiveness, and quality of
therapeutic goods, including medical devices.
• Australian Register of Therapeutic Goods (ARTG): Before a device can be
legally supplied in Australia, it must be included in the ARTG.
• Classification System: Medical devices are classified based on risk, ranging
from Class I (lowest risk) to Class III (highest risk). There’s also a separate
category for active implantable medical devices.
• Conformity Assessment: Similar to the EU, Australian manufacturers must
undergo a conformity assessment. The specifics vary depending on the
device’s classification and origin.
• Post-market monitoring: The TGA actively monitors the performance of
devices on the market, ensuring that they continue to meet safety and
performance criteria.
6. China – NMPA
• Regulatory Body: National Medical Products Administration (NMPA),
formerly the China FDA, the NMPA is responsible for supervising the safety
management of food, drugs, and medical devices.
• Device Classification: Devices are classified into Class I, II, or III based on risk.
Class III devices are the highest risk.
• Registration and Approval: All devices, regardless of classification, require
NMPA registration and approval.
• Clinical Trials: Local clinical trials and technical documentation translations
are often needed, especially for higher-risk devices.
7. India – CDSCO
• Regulatory Body: The Central Drugs Standard Control Organization (CDSCO)
is India’s primary authority for drug and device regulation. The CDSCO
regulates medical devices in India under the Drugs and Cosmetics Act.
• Device Classification: The CDSCO classifies medical devices into four risk
categories: Class A (low risk), Class B (moderate risk), Class C (high risk), and
Class D (implantable). Class C and Class D devices require premarket
approval.
• Device Registration and Licensing: Before market introduction, devices must
be registered with CDSCO, and manufacturers need licenses.
• Clinical Trials: Clinical evidence might be required depending on the device
classification.
• Import License: An additional import license is essential for foreign
manufacturers.
Conclusion
Medical device regulations are in place to protect patients from unsafe and ineffective
medical devices. These regulations vary from country to country, but they all share the
same goal: to ensure that medical devices are safe and effective for their intended use.
While this post offers a brief overview, regulatory affairs professionals are the “real
heroes” navigating these intricate frameworks, ensuring that innovations in healthcare meet the highest standards of safety and efficacy.